Observations of indoor motion patterns are analyzed in real-time to trigger actions.
Our groundbreaking digital platform collects data about the behavior of seniors in their living environment, and provides feedback about the conditions, so that the right measures can be taken to counter imminent (safety) and long-term (vitality) threats.
By organizing the feedback loop in real-time on 7/24 basis, the end user is nudged towards risk-avoiding behavior (“Health Literacy”). Understanding his risk profile is prerequisite for cooperation to targeted preventive care. This is win-win: the end user gains quality of life by countering decline. The care organization can avoid or postpone care interventions, thus optimizing its resources.
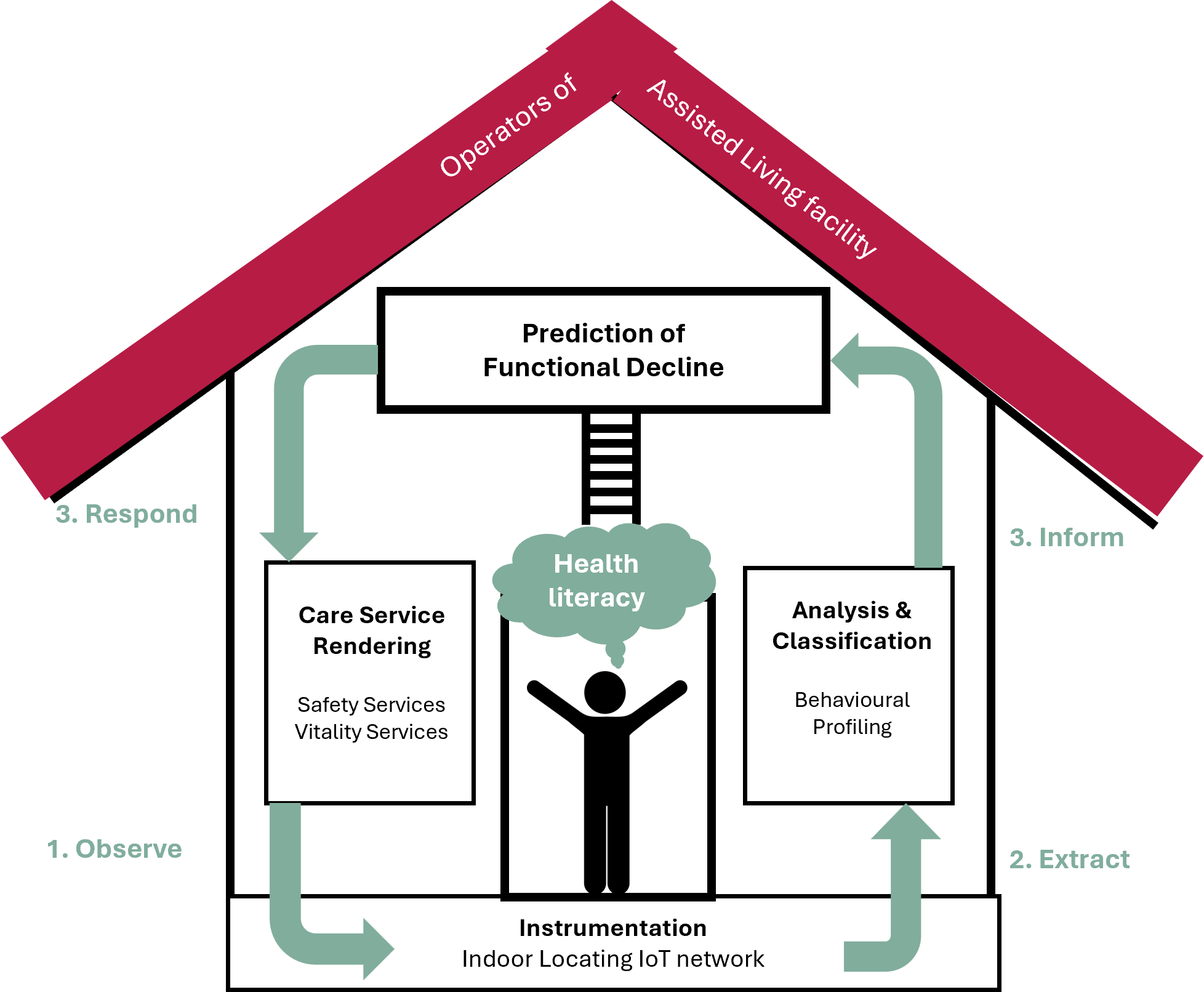
The feedback loop is given in the infographic in this page and contains four steps.
- Data acquisition (“Observations”) occurs by a IoT network (Indoor location, home automation technologies, enabled devices, wearables) that provides information on movement and body conditions in real-time.
- The observations are “extracted” from the infrastructure, and stepwise transformed into Activities of Daily Living (ADL), i.e. behavioral patterns that indicate the condition of the individuals in real time.
- Functional Decline Predictors assess the geriatric risk, either on the short term (cardiac arrest, fall) or on the long term (dementia, frailty). These predictors are AI algorithms trained on a population of elderly, taking the real-time timeseries as their input and producing risk level as their output.
- Based on these predictions, Care services “respond” by triggering automated web services in various forms, e.g. dashboarding to detect long-term decline trends, or emergency calls to counter incidents. Care Services are typically custom functions, interfaced by an API. Feedback to the end-user occurs in (automated) voice conversations, aiming to increase the resident’s health literacy.
- Changed behavior can be “Observed” – and the circle is round.
Learn more about:
